Tel: 07966 934700
Email: [email protected]

“Sexual health is the integration of the somatic, emotional, intellectual, and social aspects of sexual being, in ways that are positively enriching and that enhance personality, communication and love.
Fundamental to this concept are the right to sexual information and the right to pleasure:
(WHO 1975)
These statements from the WHO are surely just as apposite now, even in the age of Viagra, as they were over thirty years ago. Note that the WHO considered it to be a human right to be free from “psychological factors inhibiting sexual response” and from “organic disorders, disease and deficiencies”. Is it not then our duty, as clinicians in the field of sexual medicine, to ensure that our patients and their partners have these rights restored to them by our interventions?
The last few years have seen a growing recognition of the impact that sexual issues can have on the overall quality of life of patients. It is now increasingly acknowledged that sexuality is a significant and integral element of total health that must be considered in the care of all patients at all stages of various disease trajectories
It is also recognised that both diseases and their surgical or medical management can significantly affect sexual function and expression. These include cardiovascular disease, diabetes, inflammatory bowel disease, prostate cancer, and other cancers.
As with all specialist care, the clinician (following assessment) sets out objectives that are felt to be: holistic in nature; important to you; cover all aspects of the your care; and is understood and achievable by the individual.
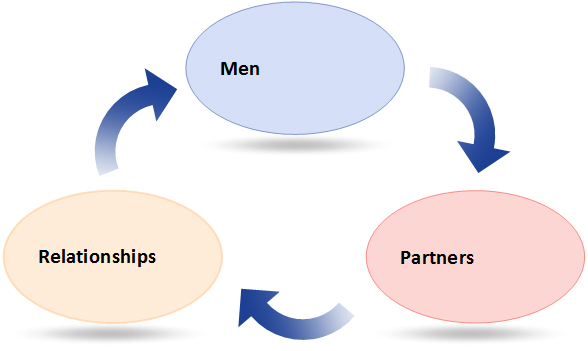
Our goal of sexual rehabilitation is to restore the your ability to engage in intimate interpersonal relationships. It incorporates the restoration of self-esteem, self concept and confidence, as well as bodily function or adaptation to physical or body image change (Bancroft 1989). When appropriate and desired, sexual rehabilitation includes restoring the physical ability to engage in sexual activity.
This will be based on the patient’s perception of their sexuality and what is important to them at that time. The key to a good outcome is improved assessment of individuals, comprehensive documentation of problems, realistic expectations of sexual outcomes, and appropriate interventions at the stage that is of most benefit to you and your relationship
The experience invariably begins before the point of diagnosis and clearly, needs can change over time. Through the identification of the issues and feelings, and by understanding what helped or hindered adaptation and coping, it is hoped that realistic expectations of sexual outcomes can be given.
Male sexual function can too easily be considered as relating purely to erectile function, but this is far from the truth. There are many possible facets to male sexual dysfunction, both physical and psychological. These include
The diagram shows some of the anatomical features of the penis that are important in erection formation.
The nervous control of penile function involves several different systems and pathways. Flaccidity or erection depend on the relative activity of the sympathetic nerves (promoting flaccidity) and a combination of parasympathetic nerves and cavernosal nerves that promotes erection.
Orgasm and ejaculation are under the control of yet different nerves, as is sensation. Therefore there are a number of pathophysicalogical issues that can interrupt the erection and the sexual response

When an erection occurs, the following happen: